Contact Us
1 Pickle Mews, London, SW9 0FJ
What’s the Appetite Among Doctors for VR in Medical Training?
Published
Jan 02, 2025
Tags
We discuss the results of Jonny’s recent study of junior doctors’ attitudes and understanding of VR in medical training.
Extended reality technology (XRT) is made up of virtual reality (VR), augmented reality (AR), and mixed reality (MR). The UK’s healthcare sector is growing its use of XRT – in part, due to the impact the Covid-19 pandemic had on time to train the workforce. It's also thanks to the adoption of remote, online learning, which has become somewhat mainstream in a sector that’s long relied on more ‘traditional’ means of training.
Yet whilst various studies (including The Topol Review) have lauded XRTs to continually develop the skillset of our surgeons, doctors, and nurses, barriers to adoption remain common. As usual, cost is a sticking point. But arguably more so is our workforce’s low understanding of extended reality technology.
Using VR in Medical Training
As it stands, XRT is most applied to medical practices like:
- Procedural step rehearsal
- Remote surgical assistance
- Emergency triage readiness training
- Robotic surgery
Healthcare professionals use the tools to practice and refine their skills in virtual experiences that don’t require the need for a patient. Nor does the activity necessarily need to take place in a medical setting. For instance, when a trainee surgeon wears a VR headset to train on an orthopaedic procedure, they can immerse themselves in the virtual theatre from anywhere.
Though more hospitals, clinics, and universities are incorporating medical VR tools in their training programmes, understanding of what the technology is disparate for students, trainees, and the wider workforce.
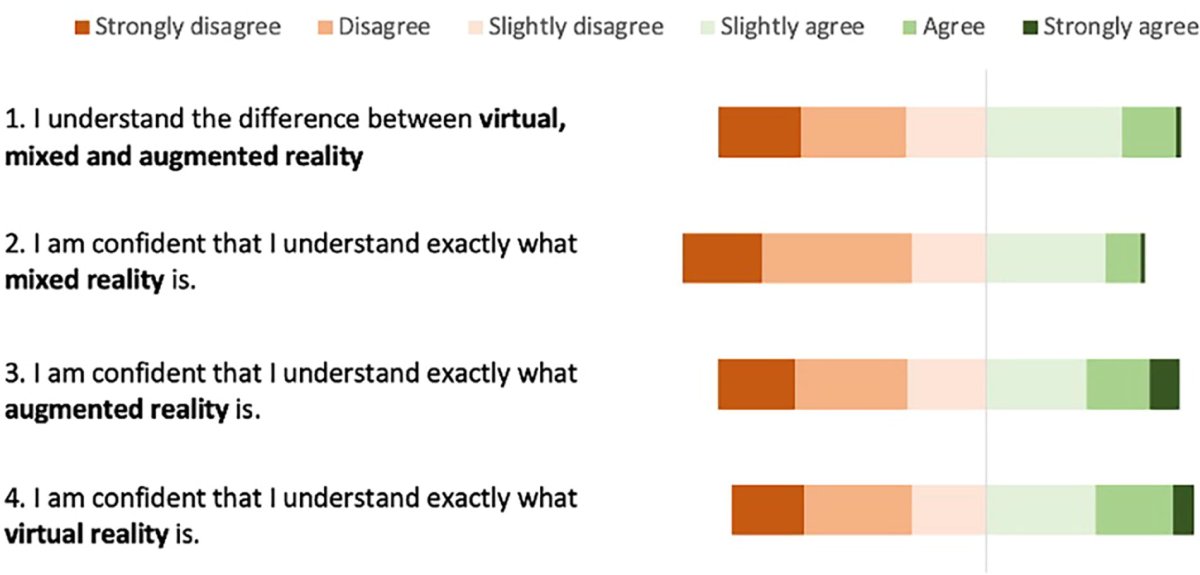
Figure 2: Summary of Likert responses for the self-assessed knowledge questions
Understanding, Experience, and Attitudes Toward Extended Reality Technology: A Multicenter Study
Exploring Barriers of Medical VR Training
In April 2024, Jonny Abbas, our Medical Director, published research that explored barriers to XRT’s adoption – which is where the above figure is taken from. His research team assessed just short of 200 junior doctors’ understanding, attitudes, and experience of XRT. Most were working at the Foundation Programme level or equivalent, such as locally employed doctors at the same level of seniority.
Top line results show a low understanding of, and experience with, XRT. Knowledge of XRT hardware was the most lacking, compared to knowledge of VR technology which was most confidently shown.
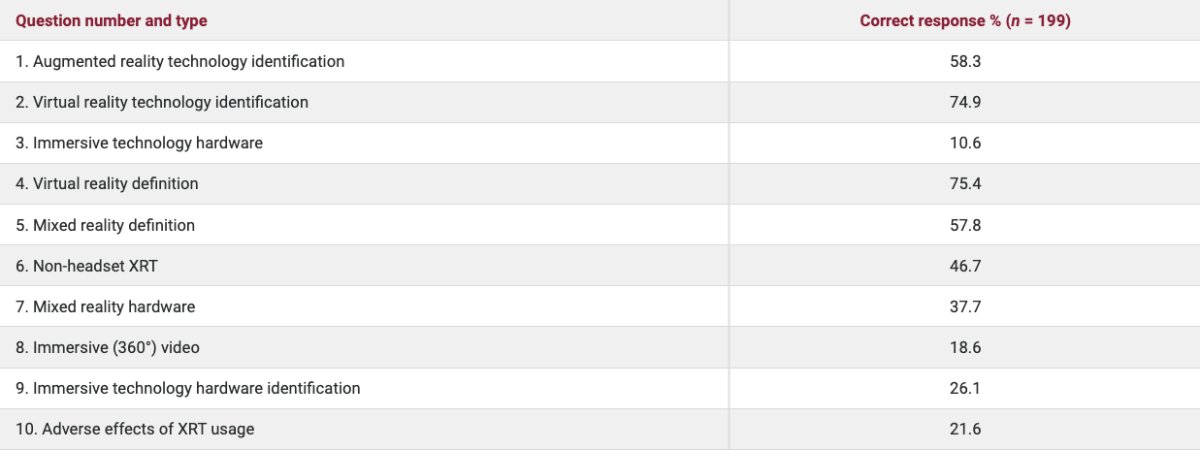
Table 3: A summary of the knowledge test and the success rate of the participants selecting the correct answer
Understanding, Experience, and Attitudes Toward Extended Reality Technology: A Multicenter Study
Despite knowledge of the hardware being low, there was considerable interest in the potential value of XRT in healthcare – particularly within junior doctor training.
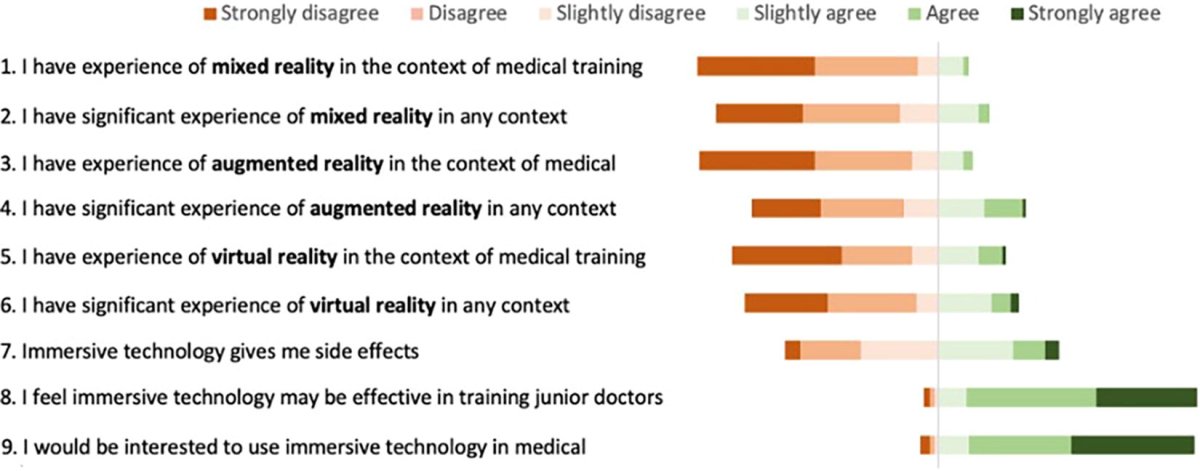
Figure 3: Summary of Likert responses to the self-assessed attitudes and experience questions
Understanding, Experience, and Attitudes Toward Extended Reality Technology: A Multicenter Study
Understanding, Experience, and Attitudes Toward XRT
Results were gathered through three assessments:
- An objective knowledge test in a multiple-choice question format
- Specific self-assessed knowledge questions in a Likert-style questionnaire
- Experience and attitudes toward the technologies were measured using self-assessed experience questions and self-assessed attitude questions
Promisingly, they found nearly all participants (93%) were interested in using XRT in their medical education. When asked if they believed it may be effective in medical training, the proportion in agreement grew to 94%.
The Future of Using XRT for Medical Training
Looking forward, the UK healthcare system is in a prime position to scale its adoption and use of XRT – for both the workforce and patients it cares for. Various virtual and mixed reality solutions are being developed and trialled, or even rolled out, to treat patients for conditions like severe agoraphobia.
Healthcare professionals are benefitting from the tools, too, for more than just skills practice or CPD. With the University of Plymouth, we’re developing a relaxation VR tool to reduce the chance of stress and/or burnout in mental health staff.
But, the rewards of VR in medical training and treatments won't be fully realised until our medical workforce are educated on, and empowered with, immersive technology digital literacy. For XRT to become mainstream in our hospitals and universities, healthcare professionals need to firstly understand its existence, and secondly, have a basic understanding of its capabilities.
With over 1.2 million staff in England, the NHS is one of the largest employers in the world. It is vital that we empower NHS staff and patients to use emerging digital technologies.
Professor Rachel McKendry
Co-Chair – Digital Medicine Panel, The Topol Review
The Topol Review
The Topol Review (2019) identified several disruptive technologies that are likely to significantly alter how we deliver healthcare – such as artificial intelligence, machine learning, and digital medicine. Government bodies have since designed formal training programmes to support clinicians’ understanding of these. Yet, no training fellowships or programmes exist for XRT, despite the technologies being cited in Sir Eric Topol’s report – and that’s a barrier to adoption in itself.
The report went on to recommend NHS organisations to ‘invest in their existing workforce’ to ‘develop specialist digital skills’. Both the assessment and commissioning of digital technologies through continuous professional development (CPD) were included in the recommendation. So, why is XRT being left out?
The Time is Now
Day in, day out, extended reality technologies are becoming more commonplace in our daily lives. The overwhelmingly positive attitudes of junior doctors in Jonny’s study makes a strong an argument for it within our medical settings, too. ‘There is no time to waste’ is The Topol Review’s closing remark, and we couldn’t agree more.
To speak to Jonny about his research findings further, or for advice on implementing VR medical training at your organisation, get in touch.
Most recent posts
Like what you read?
Please get in touch with us.



